CHAPTER NO. 1 : GENESIS OF THE MARKET
1.1 Market Prelude – Introduction & Scope
1.2 The Big Picture – Objectives & Vision
1.3 Strategic Edge – Unique Value Proposition
1.4 Stakeholder Compass – Key Beneficiaries
CHAPTER NO. 2 : EXECUTIVE LENS
2.1 Pulse of the Industry – Market Snapshot
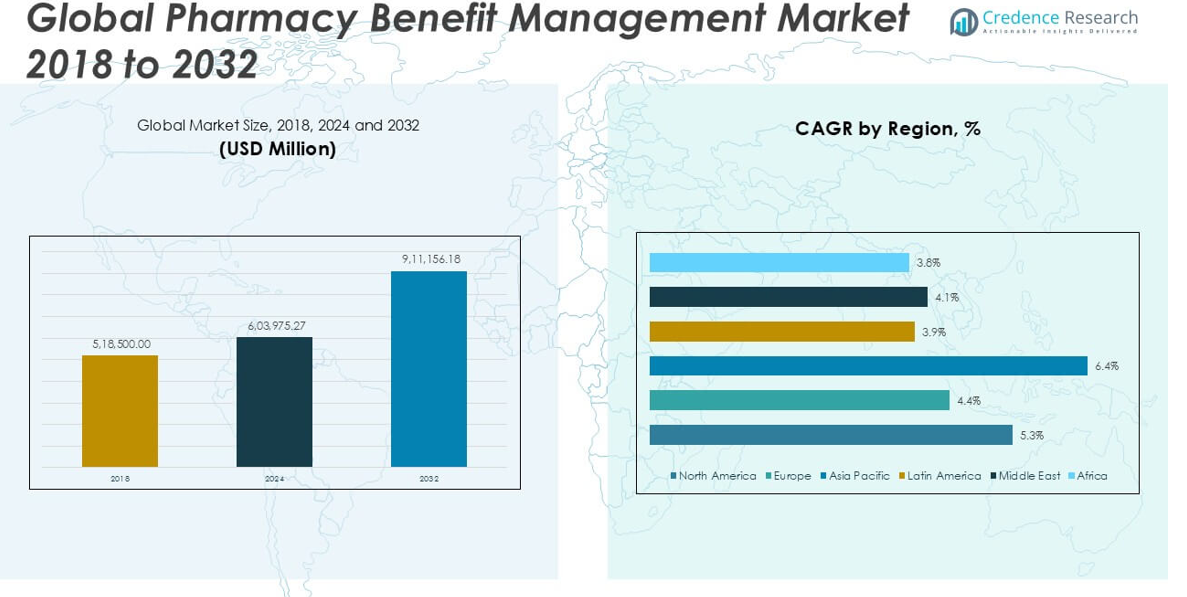
2.2 Growth Arc – Revenue Projections (USD Million)
2.3. Premium Insights – Based on Primary Interviews
CHAPTER NO. 3 : PHARMACY BENEFIT MANAGEMENT MARKET FORCES & INDUSTRY PULSE
3.1 Foundations of Change – Market Overview
3.2 Catalysts of Expansion – Key Market Drivers
3.2.1 Momentum Boosters – Growth Triggers
3.2.2 Innovation Fuel – Disruptive Technologies
3.3 Headwinds & Crosswinds – Market Restraints
3.3.1 Regulatory Tides – Compliance Challenges
3.3.2 Economic Frictions – Inflationary Pressures
3.4 Untapped Horizons – Growth Potential & Opportunities
3.5 Strategic Navigation – Industry Frameworks
3.5.1 Market Equilibrium – Porter’s Five Forces
3.5.2 Ecosystem Dynamics – Value Chain Analysis
3.5.3 Macro Forces – PESTEL Breakdown
3.6 Price Trend Analysis
3.6.1 Regional Price Trend
3.6.2 Price Trend by product
CHAPTER NO. 4 : KEY INVESTMENT EPICENTER
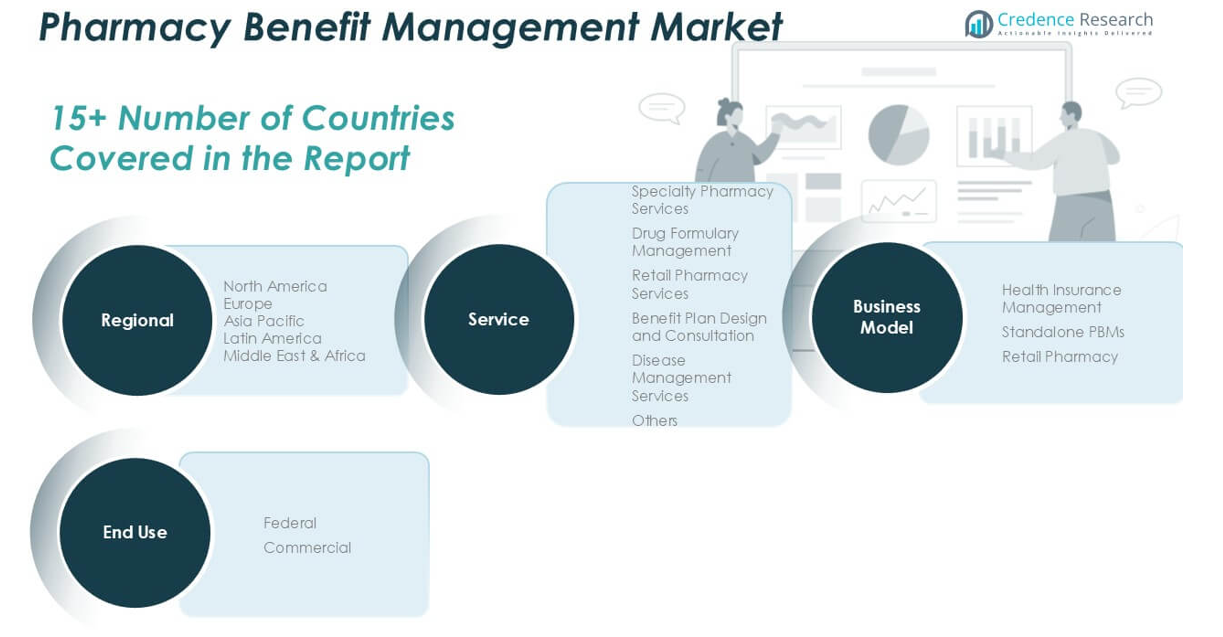
4.1 Regional Goldmines – High-Growth Geographies
4.2 Services Frontiers – Lucrative Services Categories
4.3 Business Model Sweet Spots – Emerging Demand Segments
CHAPTER NO. 5: REVENUE TRAJECTORY & WEALTH MAPPING
5.1 Momentum Metrics – Forecast & Growth Curves
5.2 Regional Revenue Footprint – Market Share Insights
5.3 Segmental Wealth Flow – Services & Business Model Revenue
CHAPTER NO. 6 : TRADE & COMMERCE ANALYSIS
6.1. Import Analysis by Region
6.1.1. Global Pharmacy Benefit Management Market Import Revenue By Region
6.2. Export Analysis by Region
6.2.1. Global Pharmacy Benefit Management Market Export Revenue By Region
CHAPTER NO. 7 : COMPETITION ANALYSIS
7.1. Company Market Share Analysis
7.1.1. Global Pharmacy Benefit Management Market: Company Market Share
7.2. Global Pharmacy Benefit Management Market Company Revenue Market Share
7.3. Strategic Developments
7.3.1. Acquisitions & Mergers
7.3.2. New Services Launch
7.3.3. Regional Expansion
7.4. Competitive Dashboard
7.5. Company Assessment Metrics, 2024
CHAPTER NO. 8 : PHARMACY BENEFIT MANAGEMENT MARKET – BY SERVICES SEGMENT ANALYSIS
8.1. Pharmacy Benefit Management Market Overview by Services Segment
8.1.1. Pharmacy Benefit Management Market Revenue Share By Services
8.2. Specialty Pharmacy Services
8.3. Drug Formulary Management
8.4. Retail Pharmacy Services
8.5. Benefit Plan Design and Consultation
8.6. Disease Management Services
8.7. Others
CHAPTER NO. 9 : PHARMACY BENEFIT MANAGEMENT MARKET – BY BUSINESS MODEL SEGMENT ANALYSIS
9.1. Pharmacy Benefit Management Market Overview by Business Model Segment
9.1.1. Pharmacy Benefit Management Market Revenue Share By Business Model
9.2. Health Insurance Management
9.3. Standalone PBMs
9.4. Retail Pharmacy
CHAPTER NO. 10 : PHARMACY BENEFIT MANAGEMENT MARKET – BY END USE SEGMENT ANALYSIS
10.1. Pharmacy Benefit Management Market Overview by End Use Segment
10.1.1. Pharmacy Benefit Management Market Revenue Share By End Use
10.2. Federal
10.3. Commercial
CHAPTER NO. 11 : PHARMACY BENEFIT MANAGEMENT MARKET – REGIONAL ANALYSIS
11.1. Pharmacy Benefit Management Market Overview by Region Segment
11.1.1. Global Pharmacy Benefit Management Market Revenue Share By Region
11.1.2. Regions
11.1.3. Global Pharmacy Benefit Management Market Revenue By Region
11.1.4. Services
11.1.5. Global Pharmacy Benefit Management Market Revenue By Services
11.1.6. Business Model
11.1.7. Global Pharmacy Benefit Management Market Revenue By Business Model
11.1.8. End Use
11.1.9. Global Pharmacy Benefit Management Market Revenue By End Use
CHAPTER NO. 12 : NORTH AMERICA PHARMACY BENEFIT MANAGEMENT MARKET – COUNTRY ANALYSIS
12.1. North America Pharmacy Benefit Management Market Overview by Country Segment
12.1.1. North America Pharmacy Benefit Management Market Revenue Share By Region
12.2. North America
12.2.1. North America Pharmacy Benefit Management Market Revenue By Country
12.2.2. Services
12.2.3. North America Pharmacy Benefit Management Market Revenue By Services
12.2.4. Business Model
12.2.5. North America Pharmacy Benefit Management Market Revenue By Business Model
12.2.6. End Use
12.2.7. North America Pharmacy Benefit Management Market Revenue By End Use
12.3. U.S.
12.4. Canada
12.5. Mexico
CHAPTER NO. 13 : EUROPE PHARMACY BENEFIT MANAGEMENT MARKET – COUNTRY ANALYSIS
13.1. Europe Pharmacy Benefit Management Market Overview by Country Segment
13.1.1. Europe Pharmacy Benefit Management Market Revenue Share By Region
13.2. Europe
13.2.1. Europe Pharmacy Benefit Management Market Revenue By Country
13.2.2. Services
13.2.3. Europe Pharmacy Benefit Management Market Revenue By Services
13.2.4. Business Model
13.2.5. Europe Pharmacy Benefit Management Market Revenue By Business Model
13.2.6. End Use
13.2.7. Europe Pharmacy Benefit Management Market Revenue By End Use
13.3. UK
13.4. France
13.5. Germany
13.6. Italy
13.7. Spain
13.8. Russia
13.9. Rest of Europe
CHAPTER NO. 14 : ASIA PACIFIC PHARMACY BENEFIT MANAGEMENT MARKET – COUNTRY ANALYSIS
14.1. Asia Pacific Pharmacy Benefit Management Market Overview by Country Segment
14.1.1. Asia Pacific Pharmacy Benefit Management Market Revenue Share By Region
14.2. Asia Pacific
14.2.1. Asia Pacific Pharmacy Benefit Management Market Revenue By Country
14.2.2. Services
14.2.3. Asia Pacific Pharmacy Benefit Management Market Revenue By Services
14.2.4. Business Model
14.2.5. Asia Pacific Pharmacy Benefit Management Market Revenue By Business Model
14.2.6. End Use
14.2.7. Asia Pacific Pharmacy Benefit Management Market Revenue By End Use
14.3. China
14.4. Japan
14.5. South Korea
14.6. India
14.7. Australia
14.8. Southeast Asia
14.9. Rest of Asia Pacific
CHAPTER NO. 15 : LATIN AMERICA PHARMACY BENEFIT MANAGEMENT MARKET – COUNTRY ANALYSIS
15.1. Latin America Pharmacy Benefit Management Market Overview by Country Segment
15.1.1. Latin America Pharmacy Benefit Management Market Revenue Share By Region
15.2. Latin America
15.2.1. Latin America Pharmacy Benefit Management Market Revenue By Country
15.2.2. Services
15.2.3. Latin America Pharmacy Benefit Management Market Revenue By Services
15.2.4. Business Model
15.2.5. Latin America Pharmacy Benefit Management Market Revenue By Business Model
15.2.6. End Use
15.2.7. Latin America Pharmacy Benefit Management Market Revenue By End Use
15.3. Brazil
15.4. Argentina
15.5. Rest of Latin America
CHAPTER NO. 16 : MIDDLE EAST PHARMACY BENEFIT MANAGEMENT MARKET – COUNTRY ANALYSIS
16.1. Middle East Pharmacy Benefit Management Market Overview by Country Segment
16.1.1. Middle East Pharmacy Benefit Management Market Revenue Share By Region
16.2. Middle East
16.2.1. Middle East Pharmacy Benefit Management Market Revenue By Country
16.2.2. Services
16.2.3. Middle East Pharmacy Benefit Management Market Revenue By Services
16.2.4. Business Model
16.2.5. Middle East Pharmacy Benefit Management Market Revenue By Business Model
16.2.6. End Use
16.2.7. Middle East Pharmacy Benefit Management Market Revenue By End Use
16.3. GCC Countries
16.4. Israel
16.5. Turkey
16.6. Rest of Middle East
CHAPTER NO. 17 : AFRICA PHARMACY BENEFIT MANAGEMENT MARKET – COUNTRY ANALYSIS
17.1. Africa Pharmacy Benefit Management Market Overview by Country Segment
17.1.1. Africa Pharmacy Benefit Management Market Revenue Share By Region
17.2. Africa
17.2.1. Africa Pharmacy Benefit Management Market Revenue By Country
17.2.2. Services
17.2.3. Africa Pharmacy Benefit Management Market Revenue By Services
17.2.4. Business Model
17.2.5. Africa Pharmacy Benefit Management Market Revenue By Business Model
17.2.6. End Use
17.2.7. Africa Pharmacy Benefit Management Market Revenue By End Use
17.3. South Africa
17.4. Egypt
17.5. Rest of Africa
CHAPTER NO. 18 : COMPANY PROFILES
18.1. Aetna, Inc.
18.1.1. Company Overview
18.1.2. Services Portfolio
18.1.3. Financial Overview
18.1.4. Recent Developments
18.1.5. Growth Strategy
18.1.6. SWOT Analysis
18.2. Centene Corporation
18.3. Cigna Corporation
18.4. CVS Health Corporation
18.5. Express Scripts Holding Company
18.6. Magellan Health, Inc.
18.7. Medimpact Healthcare Systems, Inc.
18.8 Optumrx, Inc.
18.9. Prime Therapeutics LLC
18.10 ProCare Rx
18.11 SS&C Technologies, Inc.